This post first appeared on the Mayo Clinic Social Media Network.

When Connect, Mayo Clinic’s online community for patients and families, started to grow in numbers and activity, I knew we needed to prepare for scalability. Connect is managed by a team of community moderators, who keep the community safe, respectful, trustworthy, and inclusive. While moderation is vital, there’s a lot more to strategic community management keeping us busy. We needed help on the frontlines, so I developed a volunteer program called Connect Mentors.
Who are community mentors?
Connect Mentors are active members of the community who have first-hand experience with a variety of health conditions. They are patients, lay caregivers, and family members who volunteer to participate regularly in the community, introduce members, and spread the word about Connect. They ensure Connect remains a safe, welcoming place for people to talk about their health experiences, ask questions, find support, and share information.
Mentors are:
- Patients, caregivers or family members
- Active and regular members of Mayo Clinic Connect
- Passionate about the topics they participate in
- Knowledgeable and compassionate
- Have personal health experiences to contribute to the discussions
- Available and responsive to the groups and discussions they monitor
How do you choose mentors?
I observe member behaviors in the community before they are invited to the mentor program. Are they active and participate regularly? How long have they sustained activity? Are they articulate, supportive, and resourceful? Softer skills are really important too. Do they display good “listening” skills online; in other words, do they meet the members where they are, hear what they have to say, rather than only talking about themselves?
I encourage, thank, and reward members who display the behaviors that promote a supportive and informed community. Before inviting members to become a mentor, I will often send private messages thanking them for how they respond to members. Sending a thank you with no strings attached is a good litmus test, and usually results in an increased commitment to and involvement in the community.
Those I invite to be mentors share the purpose and goals of the Connect community and its members. To paraphrase MacMillan and Chavis (1986), a healthy sense of community means the goals of members match those of the membership as a whole and members should feel they can influence and be influenced by the community. Mentors model community norms that other community members can adopt.

What do you ask volunteer mentors to do?
I do not pre-determine roles for mentors, but rather watch their behaviors and intrinsic motivations (defined by regularity and quality and type of contributions). Mentors shape their own roles, rather than receiving an assigned role. This has several benefits. People are more likely to stay committed to a role of their own choosing. They do it naturally and training is minimal. Instead, you can enhance their natural talents as the community evolves. Additionally, they may develop roles you haven’t thought of that are very beneficial to the community.
As for expected achievements, I set the bar low at first. I send suggested tasks regularly and provide ongoing coaching and tips. Sometimes they are tasks specific to certain mentor, tailored to their skill sets or the engagement levels of the group for which they are responsible.
In general, mentors:
- Welcome and support new members
- Check in on members
- Start discussions and keep them going
- Tell people about Connect within their social networks (on- and offline)
- Work with the community moderators
- Help with testing and contribute to the improvement of the community platform
More often than not, the mentors exceed my expectations.
What are the risks and how do you mitigate them?
Certainly, there can be risks, such as volunteers tipping ownership into entitlement or bringing their bias or agenda into the community. However, most risks can be avoided by setting clear expectations, encouraging desired behavior, and regularly rewarding, nurturing, and coaching.
I created a private group for volunteer mentors and staff moderators to:
- Coach, which usually comes in the form of positive example. I congratulate a job well done, point out particularly good posts or ideas they use in the community, and encourage others to mimic good practices.
- Welcome and integrate new mentors into the group.
- Make announcements of new things coming — they get sneak previews.
- Post calls for user testing, as mentors participate in conception, development, and user acceptance of new concepts, designs, and functionality for the community.
- Co-create things like copy about Connect, blog posts, and agendas for our regular mentor meetings. Anything I do for them, I do with them.

Most importantly, mentors use the private group to connect and build a deeper sense of community amongst themselves and to improve their skills as community mentors. They talk about difficult conversations they may encounter and get ideas from their colleagues. They get support from one another when they feel tapped out or need support because of their own health issues. They also share tips about promoting the community. My favorite thread is about how a mentor uses her Mayo Clinic water bottle to start conversations with complete strangers.
When I go somewhere and I carry water, I use the Mayo Clinic water bottle that Colleen “gifted” to us at the May meeting. Since I live in Michigan, people invariably look at it and ask me why I have a Mayo water bottle. This gives me the opportunity to tell them about Mayo Connect and pull from my purse one of the Mayo Connect info cards and hand it to them. ~Teresa, volunteer mentor, 3,744 posts
Don’t forget they’re patients
We practice self-care. It’s important to remember that the mentors are patients and caregivers caring for others. They occasionally have health issues that limit their participation. Mentors will take pauses and step back from the community for periods of time. Some have chosen to retire. As the community gets bigger and more active, we are increasing the number of mentors to scale our capacity, share the load and avoid burnout. We started with three mentors and have grown to 20 active mentors and seven retired mentors.
Every mentor came to Connect as a member first, usually to seek help and support. While many experience healing in helping others, it is important to remind them that they can continue to lean on other community members in times of need.
What are the benefits?
The benefits of the Connect volunteer mentor program to the community are countless. The mentors are our biggest ambassadors, not only of the community but of Mayo Clinic (and some are not Mayo patients). Ultimately, they are the target users, so their feedback on community developments are priceless and help ensure adoption of any developments to the platform and effectiveness of outreach tactics.
But most of all, mentors are people with lived experience. They are experts by experience. They connect best with their peers best because they’ve been there. You can’t have a thriving community unless people talking, supporting, and sharing real experiences and useful information and building circles of trust. The mentors foster that conversation.
The success of an online community relies on growth (new users), activity (posts and returning or alumni users), and deepening sense of community, trust, and connection. Developing and nurturing a volunteer group of peer mentors contributes significantly to Mayo Clinic Connect’s success. Just look at the growth in numbers and engagement on Connect for the past 18 months since we introduced the program.

Key takeaway
Managing a volunteer group takes time and effort. Volunteering must be rewarding for the volunteers, and you have to ensure that it is. Compensation comes in many forms. Make the time to show volunteers they are genuinely valued, appreciated, and respected. Shows the results of their work. And don’t forget, the power of “thank you” goes a long way.
By Sarah Gilbert (@_sgilbert_)
Why do people take part in online communities? I set to find out.

Sarah Gilbert
Between February and June of 2015, I interviewed 23 #hcsmca community members and founder, Colleen Young, as part of my dissertation on what drives people to participate in online communities. As a forum in which a diverse network of people who are passionate about health gather to research, discuss and problem solve challenges and opportunities in Canadian healthcare, #hcsmca is aptly described as a community of practice. Because learning is an integral aspect of participation in communities of practice, I sought to explore the role of learning as a motivation for participating in #hcsmca. I was interested in three key research questions:
- What role does learning play as a motivation for participation in the #hcsmca community?
- How do Twitter and the tweet chat format affect learning for members of the #hcsmca community?
- How is learning enacted for members of #hcsmca through their participation in the community.
To respond to these questions, I looked to the interviews for references of learning, descriptions of their experiences using Twitter and the tweet chat format as a discussion platform, and descriptions of how participants learned by participating in discussions.
The importance of learning for #hcsmca community members
Learning and participating in the knowledge exchange process was found to be a key driver for participating in #hcsmca. 17 of the 23 community members interviewed responded that learning was a driving factor of participation. Five of those who did not cite learning as a motivator cited sharing knowledge with the group as a driver for participation in the community. When directly asked, all participants indicated that they had learned through their participation in the community, although one participant could not think of an example.
Twitter and learning
Because Twitter is the medium through which most community members interact, I was interested in the impact of the platform and the tweet chat format on learning. Participants highlighted a number of ways Twitter supported discussions: it was cited as accessible, fast, efficient, and democratizing. Upon asking Colleen @colleen_young, why Twitter? She responded:
Twitter is just extremely accessible. It’s very quick. People do have some skepticism around the length of the messages that people are able to write, but there’s a lot of efficiency in keeping your comments to 140 characters. It’s a really level playing field for that as well.
And many participants agreed! For example, features such as liking and favouriting allowed a participant with a cognitive impairment to be visible and support the community when she was not well enough to participate actively in the chats. @anetto described Twitter’s democratizing effect:
It’s easier for me to meet people and talk to people online than it is to talk to them in person. I mean it seems more egalitarian doesn’t it? … You’re influenced so much by the way people look, right? And so if you’re young and vibrant and well dressed and you have great shoes, you’re going to get a different response than if you’re older and maybe a little stooped and your shoes are ugly…So I like that that’s not what happens so much on Twitter.
While most participants were supportive of Twitter as a platform to engage in healthcare discussion, six noted limitations of the technology. The most common criticism was that the chats were awkward and hard to follow; one participant described the chats as stressful so she tended to avoid them. Two participants were concerned that the 140-character limit could not support the depth of discussion they would like to see come from the community. As a supplement to the Tweet chats, a monthly in-person sub-community was founded by members in BC, Evening Rounds, and annual meet-ups were organized by Colleen with planning support from the community.
Learning through participation
The final research question was posed to identify how learning is enacted through participation in the community. Through analysis I identified four main themes: knowledge exchange between experts and novices, learning what others know, exposure to diversity, and learning knowledge they can practice.
Twenty participants cited social learning as a motivation for participation: 13 interviewees valued the opportunity to share their expertise and 17 valued the opportunity to access the expertise of other members, with some overlap between the two. Because the personal and professional experiences of the community members are so diverse, members may be simultaneously experts and novices, allowing those who are traditionally considered experts to occupy the position of novice. For example, @drpauldempsey cited learning from patients as a key motivator:
I appreciate hearing the perspectives of patients and non-doctors. So I tune in primarily because I like to listen in and get a different perspective on things. That helps me, in my view, plan services; it helps me respond to patients in the office, it helps me with what we do with our Quinte Pediatric work online. And if it’s a topic that I can additionally add some information or my input, that’s great. But I don’t go there to try to have a platform or to speak or to present, I go there to learn. Really listen and learn.
While patients, often through a drive to act as self-advocates and raise awareness, take on the role of expert, as @CatToyOriginal does when sharing information about her rare disease:
In the early days it was really scary, so that’s when I will really tweet something to hcsmca with that tag … it’s a way to keep the name of this illness out there … half the battle is … to get it talked about enough so that it’s in [doctors’] minds. Somebody walks into their office and they are struggling with all these things, [doctors] will think of it because people are talking about it.
Learning about who’s who in healthcare, and who knows what was a driver for 14 participants. This was an important professionally driven motivation for community members who are new to the field and also an important personally driven motivation for those who had specific questions about the healthcare system; for example, @eringarrity described how participation in #hcsmca helped her situate herself in the healthcare field:
I’m reading who’s writing what, when are they writing, what are their positions, opinions, and then, if I want to … I can pursue something more.
Community members expressed a sense of trust – knowing who knows what was often expressed hand in hand with a sense that community members would be willing to help and could provide reliable responses.
Access to the diversity of voices, roles, ideas, and experiences of community members was a driver for 14 participants and was something that they highly valued; in the words of @kathykastner:
The fact that I have this worldwide pool of brains that I can call upon and will answer me is like gold!
Several participants expressed the the community was the only way that they would have access to a diverse network of people and therefore access to a range of information. For example, @pat_health described the unique advantages he gets from the community:
At the micro level I get insights into projects and perspectives that I wouldn’t otherwise have any knowledge of, especially in Canada. I get more insight into various aspects of the community or groups in the community, like the engaged patients and the other health professionals, the PR people that are working for hospitals. I gain a lot of insights into where people are coming from so the value I get from it ranges from very specific topics and areas.
While generally the community was discussed as diverse, several community members (in an interview and during the chat I hosted, see for a link to the transcript) were concerned that while the group was diverse, their similar values led to topics discussed in an echo chamber.
In discussing learning through participation in the community, eight participants noted that they had been able to apply what they’d learned. For example, two physicians, including @drpauldempsy, cited above noted that they were able to improve their practice applying what they’d learned through the community. Others learned leadership skills through planning events and moderating chats, and others, such as @DrRKSingal were able to learn the norms and conventions of tweeting as professionals:
I used it as a way early on just to learn simple things: you know, how do professionals conduct themselves on Twitter. I mean, a tweet chat is a very good way to kind of figure out what your own style might be; what’s kosher, what’s not. I actually modeled a lot of it after the way Colleen conducted herself, you know. So I learned a lot from her actually.
@SaraHamil noted that participation in the community provided her with information that she could use in her personal life:
I feel much better equipped that, should the time come where I need to be more involved in my own health, I feel like I’m better equipped with the tools that I need than had I not participated in the community.
In the analysis I teased apart the four themes; however, each of these aspects of learning affects the other: for example, learning who knows what provides members with information about the knowledge of an array of experts who have diverse areas of expertise. Knowledge learned through these interactions may then be put into practice. In viewing the themes as interwoven, the rich tapestry of learning through participation in #hcsmca emerges.
#hcsmca-ers, I’d like to know what you think! Do my findings align with your learning experiences? Why or why not?
A full report of my findings can be found here (paywall): http://www.tandfonline.com/doi/abs/10.1080/1369118X.2016.1186715?journalCode=rics20
If you do not have access to the paper and would like to read it, please email me at sagilber@mail.ubc.ca for a link to an e-print.
Chat Summary 250: #RareDiseaseDay: Do stories change anything?
By Emma Rooney (@blumencasey)

On February 3rd #hcsmca explored how stories can change things. We asked
- T1. How do patient stories impact the rare disease community?
- T2. How can we better value patient stories and respond to the insights shared?
- T3. What benefits should patients look for from contributing their stories?
- T4. What stories are missing from the rare disease community and how can we encourage different voices?
Here’s the Storify of our discussion.
@drpauldempsey 20 years ago, my story didn’t matter, I was told what to do. I love the change now since I’m asked what I need next. #hcsmca
— Martin R. Lemieux (@martin_lemieux) February 3, 2016
CT Seek out stories that on the surface are not similar to our own and then look for the connections and commonalities #hcsmca
— Pam Ressler (@pamressler) February 3, 2016
@hcsmca Ct: I want everyone in the rare community to have a voice, to have a place at the table. We are stronger together. #hcsmca
— Tattered Edge (@tatterededge) February 3, 2016
Read the complete #hcsmca chat 250 transcript.
#hcsmca: 5-year Retrospective and Looking Ahead
It’s been an amazing 5-year journey with #hcsmca. Here’s the retrospective that I shared at the #hcsmca Symposium on Feb 24, 2016. (Slides)
Who would’ve ever thought that 140 characters could change an industry? Health care is an industry built on science, art, evidence and communication. But the social Web and the networks we build are causing a paradigm shift in how health interactions are perceived.
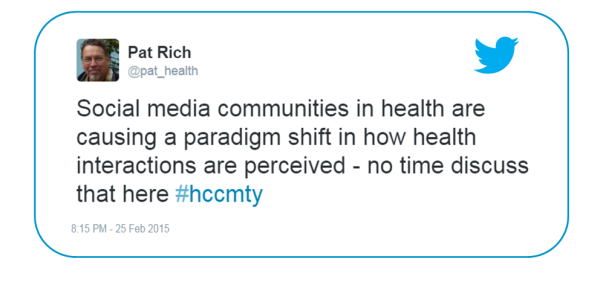 Pat Rich said this exactly a year ago at the 2015 #hcsmca Meetup in Toronto. But look at the last part of the tweet. “No time to discuss that here.” Today, we have time. Today that’s why we’re here – in person and online.
Pat Rich said this exactly a year ago at the 2015 #hcsmca Meetup in Toronto. But look at the last part of the tweet. “No time to discuss that here.” Today, we have time. Today that’s why we’re here – in person and online.
Five and a half years ago, when social media were still quite new to most people in health care, I established the hashtag #hcsmca – Health Care Social Media Canada. While the first #hcsmca tweetchat was held in September 2010, the journey began weeks before.
I set out purposely to build a community. An inclusive open network of people who share a strong common interest, interact online and form relationships. First step: invite key first followers, people who would ensure that the community had a healthy mix that would model the inclusiveness and diversity I wanted this community to be built upon.

I contacted people in my offline and online networks across the country from all walks of health care – patients, providers, communicators, educators, researchers, KT specialists and so on. If I wanted to attract multiple stakeholders and wide geographic representation to #hcsmca, then representatives of those people had to be the first adopters.
Remember this was 6 years ago when there were few clinicians or organizations on Twitter, and even fewer patients and caregivers.
Already by the second wildly successful chat I started to think, Wow we’ve gone from fledgling to a flourishing community in just 2 weeks.
Still I was rather surprised when Ujjal Dosanjh, former Minister of Health joined in and submitted this topic: How can social media help caregivers find good/solid advice when they need it most? Conversation about caregiver needs, usage of social networks and criteria for “solid advice” ensued. I’m not sure what the Liberal party had hoped to gain by participating in #hcsmca, but they definitely got plenty to listen to. @ujjaldosanjh’s final post before leaving for question period read: “this forum proves there are a lot of ideas out there. Great info to share with my #LPC colleagues esp when talking w constituents.”
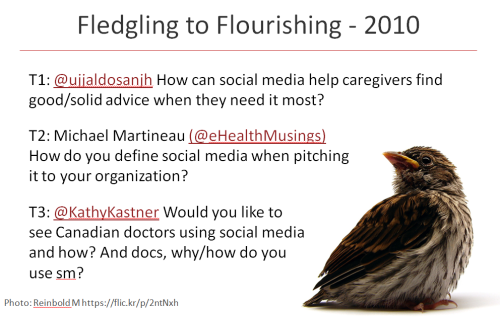
That same week the other 2 topics were submitted by Mike Martineau and Kathy Kastner, an IT specialist and a patient. This was the format of the chats for the first 2 years. People submitted their topic or question to a open Google spreadsheet; one topic per person, 3 topics per topics per week.
Six months in and #hcsmca was meeting its goal, making health care more open and connected. We were getting noticed outside the social media vacuum too. Canadian Press wrote this piece that was syndicated across Canada.

Being included in the free public transit paper in several urban centres, #hcsmca-ers heard from their colleagues, friends and family – Is this what you’ve been talking about?
You bet it is. Let’s look at the numbers. Since 2010 we’ve had
- over 90,000 participants
- contributing 220,000 tweets
- in 252 chats,
- hosted by 95 moderators.
Offline events strengthen the the sense of community of an online network. Robyn Sussel recognized this when she and colleagues started Evening Rounds – a monthly meetup here in Vancouver. In Toronto, we’ve hosted 8 meetups of over 100 people, each event using a different format from panel discussion to speed dating to Pecha Kucha competitions. Today is the first full day event! Thank you Quality Forum for inviting us to be one of 3 pre-forum events!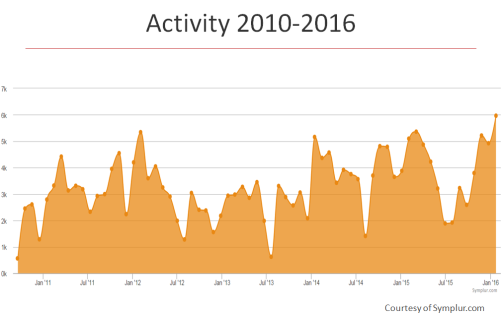
When #hcsmca was 2 years old, Anatoliy Gruzd and Caroline Haythornthwaite did a social network analysis sampling one month – November 2012.

I was thrilled with the picture this revealed: a well connected network with no central figure of influence. Meaning #hcsmca is not an audience, not a gathering, but rather an well distributed community of practice, sharing knowledge and expertise. The researchers’ analysis showed there was “no preferential attachment among people in the same professional group, indicating that the formation of connections among community members was not constrained by professional status.”
It indicates a healthy sense of community where members have a feeling of belonging
and identity. The goals of members match those of the membership. Members feel they can influence and be influenced and that they share a history, experience and/or an emotional connection.[McMillan and Chavis, 1986]
It was because of #hcsmca’s strength of community that I was asked to contribute an essay in Mayo Clinic’s book “Bringing the Social Media Revolution to Health Care” called Twitter Chats Build Community.

Every community has a lifecycle from inception, to establishment to maturity – many stay in this stage for years – and for some there’s a mitosis or death. As #hcsmca moves through its lifecycle, it’s been imperative to stay relevant, to evolve with the community, acknowledge and enable the roles people take on and challenge the collective into areas where they may not have thought to venture.
The first role that I was keen to enable was born out of necessity. It’s a lot of work to moderate a chat every week. So I invited people to help out. Over 95 people have moderated #hcsmca.

By the 3rd year, I changed the model of 3 questions from 3 people to make each chat based on a theme so we could dive deeper into a topic. The host would choose a theme for the chat, write a preparatory blog which brought focus and depth to the conversations. Another role that emerged were the summary creators. While there is a transcript for every chat, the summaries are short commentaries, infographics, storify’s. Other roles include the welcome wagonners, the data collectors, the event planning committee members and my moral supporters.
And then there are special projects. Take for example the revision of #hcsmca’s vision and mission. Last year, Shirley Williams along with Pat Rich and myself, led this incredible online consensus building initiative. For as #hcsmca grew and matured, and social media became practically ubiquitous, hosting a community focussed exclusively on social media no longer made sense and the scope was expanded to social collaboration for better health and health care.
Every #hcsmca chat shifts the needle in our understanding, perception, practice and empathy; sometimes a little, sometimes a lot.
Elise Bradt from the Council of Academic Hospitals of Ontario wrote to me after their chat about patients and research, “we are very proud and just delighted at the response we’ve received. In fact, I met with Dawn Richards the next day and we took much of our conversation from the chat into the real world, discussing CAHO’s 2015-2020 commitment to driving best practices for patient co-design of research. In my mind, this transition of dialogue (from virtual to actual) is the very purpose of the #hcsmca community.”
Patients and caregivers have also hosted chats. Annette MacKinnon and Natrice Rese co-hosted chats about online vs. in-person patient support services and health advocates.
I, too, have brought the #hcsmca community knowledge with me to Medicine 2.0 in Boston and London, and flipped my MedX panel twice with you before going to Stanford Medicine X 2014 and 2015.
#hcsmca is a safe and trusted place to test out new ideas. Members know they have a community of people encouraging them to be innovative and to take risks; one that will applaud successes and help missteps become learning opportunities.
All of the 252 chats and their respective blogs are archived – an incredible treasure trove of data.
In my opinion the single biggest achievement of #hcsmca has been to help people step back from their own area of expertise. When moderators submit their topics, often their questions need to be reframed to include everyone. While their goal may be to specifically get patient opinion or to feedback from physicians, I remind them that #hcsmca is a diverse and inclusive community and this has to be reflected in the questions. This is how #hcsmca dismantles health care’s silos and help creates pathways to connection – connections that less than a decade ago were thought impossible.
For the past 5 and half years, 70-100 people have gathered weekly, over 90,000 in total, making real connections, recalibrated their thinking and opening their minds. Yes, we can improve health care 140 characters at a time.
However, the time has come for me to take a bow. Starting in March, I will no longer be leading weekly tweetchats. But this is not the end of #hcsmca. The hashtag will live on. Today, I invite you to take up the #hcsmca baton and help create the road map of the next part of our evolution.
Thank you!
National #hcsmca Symposium Blog Roundup
Here’s everything we’ve organized and written about the #hcsmca Symposium so far. Big thanks to the entire Planning Committee Marina Bastawrous, Toronto; Janelle Chung, Vancouver; Colin Hung, Toronto; Isabel Jordan, Squamish BC; Lori Last, Vancouver; Leah Lockhart, Vancouver; Trish Paton, Edmonton; Pat Rich, Ottawa; Kevin Smith, Vancouver; Robyn Sussel, Vancouver; and Colleen Young, Toronto.
How to Unconference & the Challenges
- Submit a Challenge: Make the #hcsmca Symposium Relevant to You by Colleen Young
- How to Unconference #hcsmca Style by Colleen Young
- Vote for your favorite #hcsmca Symposium Challenges by Colleen Young
- How to Prepare for the Unconference Part of the #hcsmca Symposium by Colleen Young
- 10 Tips for Unconference Facilitators by Pam Ressler and Colleen Young
Speakers and Program
- #hcsmca to Host a National Symposium – Come with us to #QF16
- Meet the Powerhouse Panelists for #hcsmca Symposium
- #hcsmca Symposium Program & Speakers
- How to take part in the #hcsmca Symposium remotely by Trish Paton
- The livestream

Why a National Symposium
- #hcsmca Time to Take a Bow by Colleen Young
- #hcsmca National Symposium in Vancouver: The Last Waltz by Pat Rich
- #hcsmca: The Last Waltz (or … Not Last Tango in Vancouver) by Pat Rich
- #hcsmca: The Not so Hidden Agenda by Pat Rich
Patients Included (Caregivers and Students too)
- Announcing Scholarship Applications for #hcsmca’s National Symposium by Trish Paton
- Why the #hcsmca Symposium is Patients Included by Isabel Jordan
- Announcing the National #hcsmca Symposium’s Scholarship Winners by Colleen Young
Why Vancouver
- National #hcsmca Symposium Lands Out West: Why Vancouver? by Robyn Sussel
- Join the #hcsmca Symposium Dine-Around Feb 23 by Kathy Kastner

Photo credit: Michelle Preston, BC Patient Safety Learning System
How to take part in the #hcsmca Symposium remotely
By Trish Paton (@trishpaton)
You can’t make it to Vancouver for the #hcsmca Symposium? That’s OK. We would love to see you, but we know it can’t work for everyone. And we can’t fit all of #hcsmca in one room, anyway.
We’ve been planning on ways to participate if you can’t be here in real life. Here’s a few ideas you can use.
- First, download the #hcsmca Symposium Program (pdf)
- Join the livestream (www.youtube.com/embed/RdJcExxQrW0) as we broadcast mainstage from 8:45-11am Pacific time (Find your time zone.). Tweet the link!
- Follow the #hcsmca hashtag all day.
- Tweet @hcsmca a question with you’d like to ask the panel between now and Feb. 24, and we will get some of those questions into the morning.
- You can tweet questions throughout the day, too. We may not get to all of them, but we will do what we can! Make sure to use #hcsmca so we can find them.
- Stay on the #hcsmca channel for the day. We’re encouraging Challenge teams to have tweeters in the room, so a wider audience can participate.
- We are asking Challenge teams to use Google Docs to take live notes from sessions
 Be sure to follow along and tweet #hcsmca. A FitBit ChargeHR will be given to the top #hcsmca Symposium tweeter (whether you attend in person or remotely). Prize donated by @telushealth.
Be sure to follow along and tweet #hcsmca. A FitBit ChargeHR will be given to the top #hcsmca Symposium tweeter (whether you attend in person or remotely). Prize donated by @telushealth.
After the conference, everything we can get our hands on or take pictures of will be uploaded for the whole #hcsmca community to share. We encourage the Challenge teams to continue their work past Feb. 24th and to report back their progress (both what worked and what didn’t).
See you online!
#hcsmca Symposium Program & Speakers
On Feb 24, 2016 in Vancouver, #hcsmca will host its first National Symposium.
Download the #hcsmca Symposium Program (PDF).
Speakers
Robyn Sussel (Symposium Moderator), @robynsussel, Principal, Signals

Robyn has devoted her career to helping health and research organizations communicate their often hidden but compelling stories.
As one of two principals at digital firm, Signals.ca, Robyn leads the client services team and speaks regularly on the subject of health and research communications and knowledge translation as well as digital transformation and integrated communications strategy and planning.
In 2015 Robyn won the International Association of Business Communicators (IABC) Ripple Effect award for her contributions to health charities. In 2016, she was nominated for the YWCA’s Women of Distinction Award in the Health and Wellness category, again for her contributions to health and human rights charities.
Pat Rich, @pat_health, Senior Medical Writer and Editor, Commentator on Canadian Health Care
 Pat Rich is a veteran medical writer and editor and commentator on social media in the context of health care. He has been editor-in-chief of Canada’s only newpaper for physicians and recently parted ways with the Canadian Medical Association after serving for 14 years in a variety of senior communications positions including as publisher of the Canadian Medical Association Journal
Pat Rich is a veteran medical writer and editor and commentator on social media in the context of health care. He has been editor-in-chief of Canada’s only newpaper for physicians and recently parted ways with the Canadian Medical Association after serving for 14 years in a variety of senior communications positions including as publisher of the Canadian Medical Association Journal
Colleen Young, @colleen_young, Founder, #hcsmca, Online Community Director, Mayo Clinic Connect
 Colleen Young (@colleen_young) is an internationally recognized expert in building online health communities that thrive. She is the Founder of Health Care Social Media Canada (#hcsmca) – an inclusive, cross-disciplinary community driving social collaboration for better health and health care. She is also the Community Director of Mayo Clinic Connect, an online patient community.
Colleen Young (@colleen_young) is an internationally recognized expert in building online health communities that thrive. She is the Founder of Health Care Social Media Canada (#hcsmca) – an inclusive, cross-disciplinary community driving social collaboration for better health and health care. She is also the Community Director of Mayo Clinic Connect, an online patient community.
In 2012, Colleen was awarded the Journal of Medical Internet Research Award at the Medicine 2.0 Congress at Harvard University for her leadership in developing best practices for building online communities. She frequently speaks and writes about the impact of social web in health and health care, including presenting at Stanford Medicine X 2014 and 2015.
Kicking off the event is a powerhouse panel with Lee Aase, Larry Chu, Colin Hung and Isabel Jordan. Each of the panelists have built silo-busting communities in health. On Feb 24, we’ll bring them together on stage and learn more about their communities, the labours, trials, successes and how they are each making a difference in health care now and their plans for the future.
The Panelists
Lee Aase @LeeAase, Director, Mayo Clinic Social Media Network
 Lee Aase is the Director of the Mayo Clinic Social Media Network, which provides training resources, educational and networking events and a collaboration platform for healthcare communications professionals and medical providers, as well as patients and caregivers who want to safely and effectively apply social and digital strategies to fight disease, promote health and improve health care.
Lee Aase is the Director of the Mayo Clinic Social Media Network, which provides training resources, educational and networking events and a collaboration platform for healthcare communications professionals and medical providers, as well as patients and caregivers who want to safely and effectively apply social and digital strategies to fight disease, promote health and improve health care.
By night, Lee is Chancellor of Social Media University, Global (SMUG), a free online higher education institution that provides practical, hands-on training in social media for lifelong learners. In 2013, he was inducted into the Healthcare Internet Hall of Fame, and in 2014 he was appointed to a two-year term on the World Economic Forum’s Global Agenda Council on Social Media. He also was named to the list of “20 People Who Make Healthcare Better” by HealthLeaders Media.
Prior to joining Mayo Clinic in 2000, Lee spent more than a decade in political and government communications at the local, state and federal level.
Larry Chu, MD, MS @larrychu, Associate Professor of Anesthesia, Stanford University School of Medicine; Executive Director, Stanford Medicine X
 Larry Chu is a practicing anesthesiologist who runs the Anesthesia Informatics and Media (AIM) lab at Stanford University. He is an associate professor of anesthesia on the faculty of the Stanford University School of Medicine. Dr. Chu teaches three courses at Stanford University, Engage + Empower Me (a patient engagement design course) and Design for Health (applying design innovation to improve healthcare) and Medical Education in the New Millennium (challenges and opportunities for innovation and digital disruption). He collaborates with researchers in simulation and computer science at Stanford to study how cognitive aids can improve medical team performance in a crisis. Dr. Chu has received several NIH grants to study opioid-induced hyperalgesia.
Larry Chu is a practicing anesthesiologist who runs the Anesthesia Informatics and Media (AIM) lab at Stanford University. He is an associate professor of anesthesia on the faculty of the Stanford University School of Medicine. Dr. Chu teaches three courses at Stanford University, Engage + Empower Me (a patient engagement design course) and Design for Health (applying design innovation to improve healthcare) and Medical Education in the New Millennium (challenges and opportunities for innovation and digital disruption). He collaborates with researchers in simulation and computer science at Stanford to study how cognitive aids can improve medical team performance in a crisis. Dr. Chu has received several NIH grants to study opioid-induced hyperalgesia.
Dr. Chu is also the Executive Director of Stanford Medicine X, a project of the Stanford AIM Lab. Medicine X is a catalyst for new ideas about the future of medicine and health care. The initiative explores how emerging technologies will advance the practice of medicine, improve health, and empower patients to be active participants in their own care. The “X” is meant to encourage thinking beyond numbers and trends—it represents the infinite possibilities for current and future information technologies to improve health.
Colin Hung @Colin_Hung, Director of Marketing, Stericycle Communication Solutions
 Colin Hung leads the marketing efforts at Stericycle Communication Solutions, a division of Stericycle Inc that is dedicated to strengthening patient engagement through better communication. He is a true believer in healthcare technology and has been working for over 15 years at various #HealthIT companies.
Colin Hung leads the marketing efforts at Stericycle Communication Solutions, a division of Stericycle Inc that is dedicated to strengthening patient engagement through better communication. He is a true believer in healthcare technology and has been working for over 15 years at various #HealthIT companies.
In 2015, Colin was named one of the Top 20 HealthIT bloggers and one of the Top 100 healthcare Tweeters. He also served as a social media ambassador at the 2015 Healthcare Information and Management Systems Society (HIMSS) conference and 2015 Mayo Innovation Transform conference. Colin co-founded the Healthcare Leadership online community (#hcldr, www.hcldr.org), one of the most popular and active in healthcare.
Colin received an honours BA in Applied Science from the University of Waterloo and is a registered Professional Engineer in the province of Ontario. He speaks and writes regularly about healthcare, technology, marketing and leadership. Sadly Colin still cheers for the Toronto Maple Leafs, his hometown team.
Isabel Jordan @seastarbatita, Chair, Board of Directors, Rare Disease Foundation
 Isabel Jordan is Board Chair and one of the founding members of the Rare Disease Foundation. The Foundation funds care-focused research that is informed by the priorities of the rare disease community and connects families touched by rare disease. This creates a network of families, patients, health care providers, researchers and volunteers that together are working towards the same goal of making a better future for the rare disease community. Isabel is the facilitator for the Rare Disease Foundation’s Vancouver Parent 2 Parent Resource Network and helps to lead the growth of connected Resource Networks across Canada.
Isabel Jordan is Board Chair and one of the founding members of the Rare Disease Foundation. The Foundation funds care-focused research that is informed by the priorities of the rare disease community and connects families touched by rare disease. This creates a network of families, patients, health care providers, researchers and volunteers that together are working towards the same goal of making a better future for the rare disease community. Isabel is the facilitator for the Rare Disease Foundation’s Vancouver Parent 2 Parent Resource Network and helps to lead the growth of connected Resource Networks across Canada.
Thirteen years into the journey of parenting 2 children, one with a rare disease, has taught her many lessons – one of the biggest is that building community can provide care, support, resources and answers. Connecting with other parents and health care providers in the rare disease world has made her a strong proponent of patient advocacy and family- and patient-led care. These life lessons have ripples far beyond the rare disease community. Patient engagement and building community aren’t buzzwords, they are the pathway to creating a better health care system.
The stunning plenary panel is only one reason not to miss this event. Take a look at the exciting program outline, tapping in to our collective knowledge. We’ve designed a day to explore how digital communications impact quality of care, support patient-provider co-design, contribute to research and knowledge translation, and lead to interdisciplinary decision-making.
Join the #hcsmca Symposium Dine-Around Feb 23
By Kathy Kastner (@kathykastner)
 No need to dine alone the eve before the #hcsmca Symposium.
No need to dine alone the eve before the #hcsmca Symposium.
I’ve had such fun at conferences when a pre-conference dine-around was arranged. So, I’m going with the Nike slogan “Just do it” and am coordinating one for the #hcsmca National Symposium.
How it works
Sign your name to the restaurant of your choice in this Google doc. The sign-up sheet also includes and addresses of each restaurant. They are all within walking distance of the conference hotel The Hyatt Regency 655 Burrard St, Vancouver.
Meet in hotel lobby at 5:45pm on Tuesday, February 23. (Eat time is 6pm to accommodate the Eastern time zone-ers.) We’ll head to our respective meet ‘n eats for a get-to-know you IRL (in real life).
Here’s the list of restaurants to choose from. No special menu just special people. In case it’s not obvious, you pay your own way.
Reservations are under my name – Kathy Kastner.
- Cactus Club – top notch turf n surf (note 18% gratuity added to groups of 8+)
- Grain Tasting – lounge in hotel for drinks and appies ‘Dedicated to local growers’
- Royal Dinette – ‘farm to table’ The only location with a specific menu for groups of 8+ Example of a menu is in the Google Doc.
- Mosaic Grill – the hotel restaurant
- Sala Thai
- Italian Kitchen
- Copper Chimney – Indian
- Kamei – Japanese/Sushi
- Victoria Chinese
Sign-up here to join us. See you Tuesday!
How to Prepare for the Unconference Part of the #hcsmca Symposium
Are you ready for the National #hcsmca Symposium? What do you need to know? Start by reading How to Unconference #hcsmca Style.
Unconferences are events run by participants. Attendees submit topics, set the agenda, lead the sessions and create an environment of innovation and productive discussion.The unconference part of the day is divided into 4 parts (See the program):
- Building the Wall – Instructions & introducing the challenges & making new ones
- Discovering Solutions – Breakout sessions (50 min.)
- Consolidate & Formulate Your Ideas – Action plan (40 min)
- Solutions Exchange – Report back (2 minute presentations)
1. Building the Wall
This is where attendees set the agenda. On the wall there will be the 12 challenges that you submitted and voted for in the week leading up to the conference. There’s also room for more sessions. If there’s a burning question or challenge that you would like to lead, add a wildcard challenge on the day of the symposium.
Principles of an unconference
- If you submit a topic, you lead the discussion.
- The people who show up to your session are the right people.
- Whatever happens is what was meant to be.
- The ideas put forward are the right ideas.
Law of two feet: Follow your interest. If you find yourself not learning or contributing at any time, move to a discussion where you can learn and contribute.
Once the sessions have been presented and wall is built, participants will go to their session locations.
2. Discovering Solutions
In this 50-minute session, the facilitator will
- Ask you to introduce yourself with your name only
- Elect a note take and timekeeper
- Restate the session topic and what s/he hopes to get out of the session. Frame it in the form of a question to the group (1 minute)
Read more about facilitating an unconference session in this #hcsmca Symposium – Facilitator Quick Reference and 10 Tips for Unconference Facilitators.
The facilitator will keep the conversation moving and ensure that everyone has a chance to speak. Participants should “speak up and step back,” meaning share your idea and then let others speak. Be careful not to dominate the conversation.
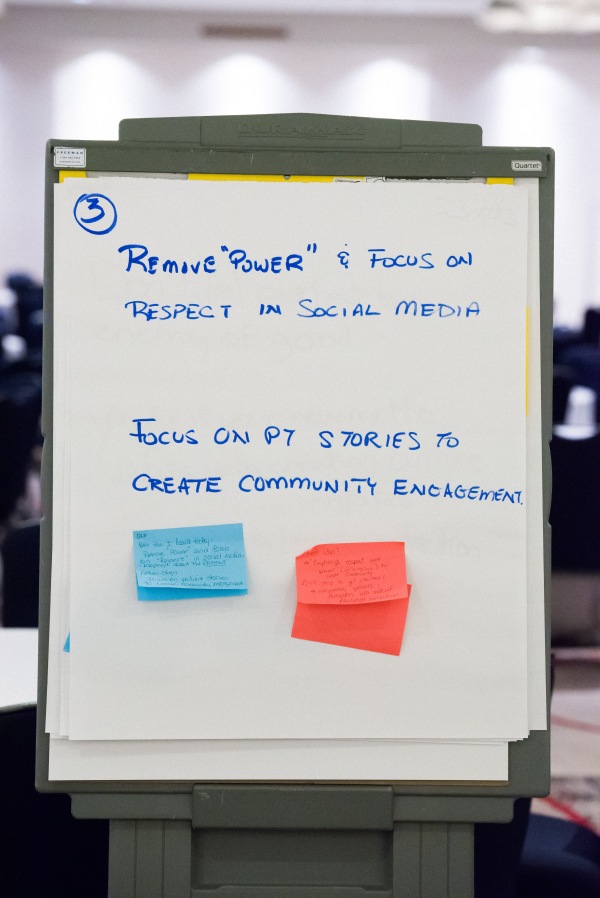
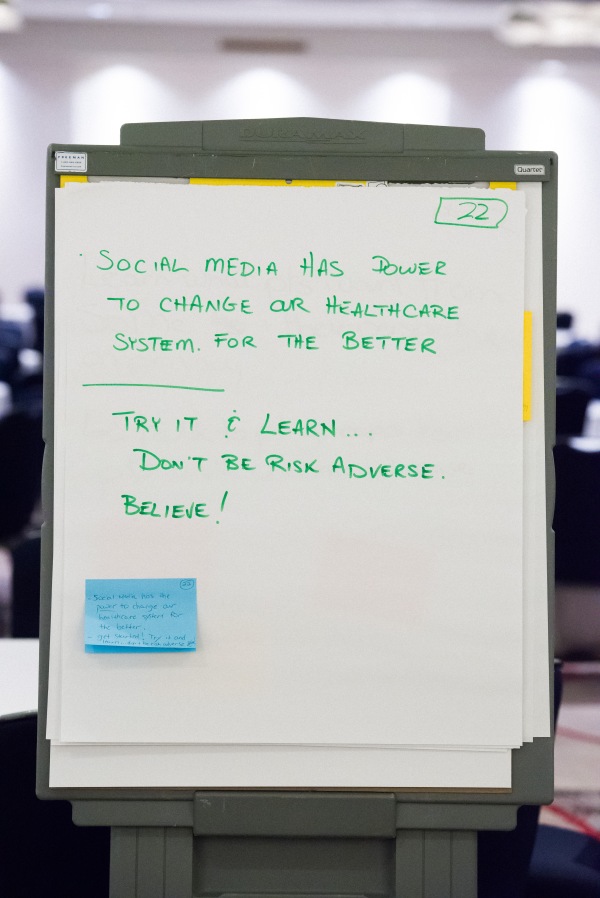
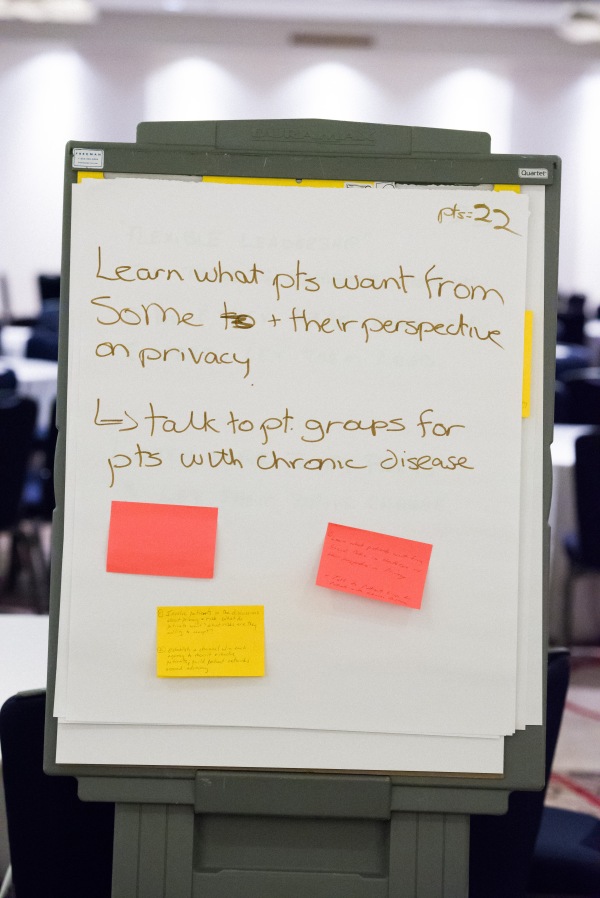
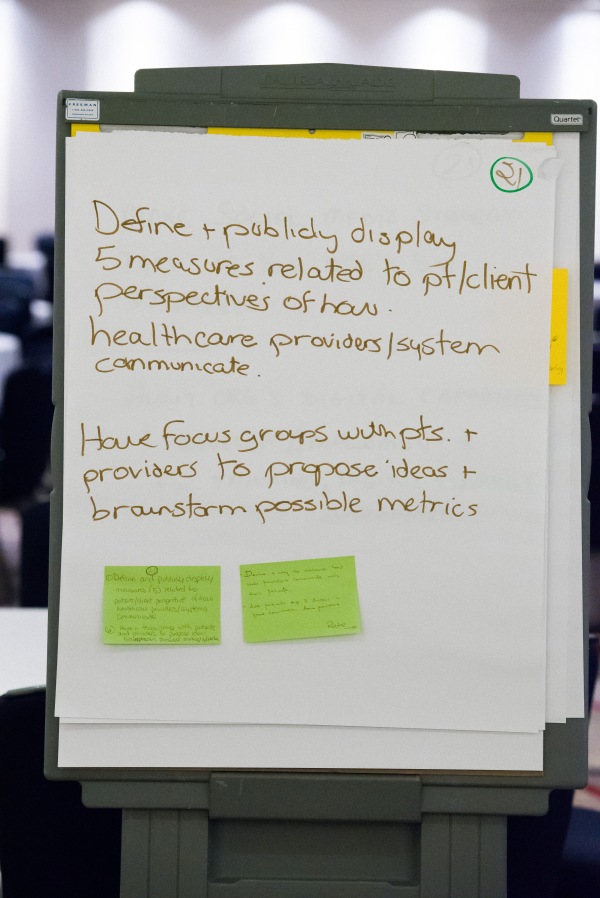
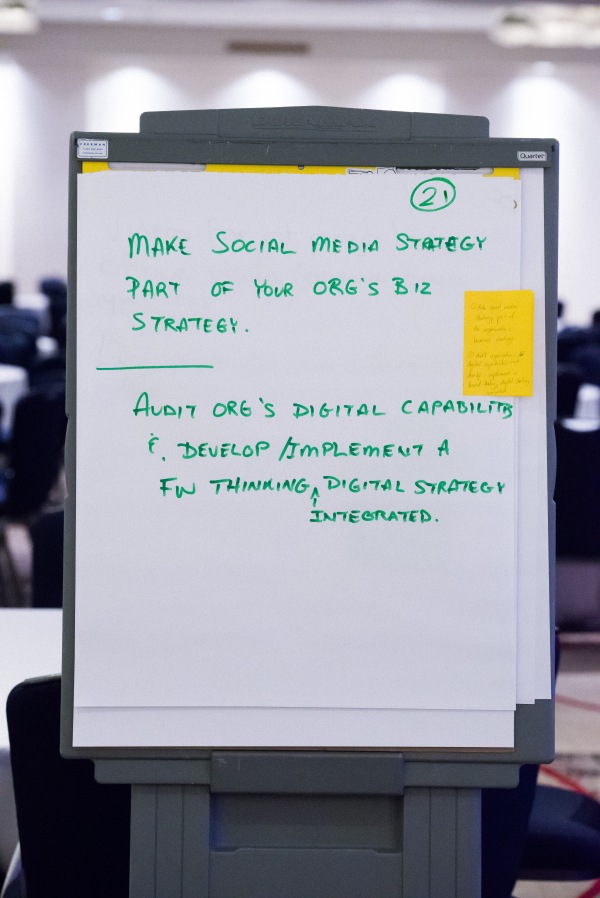
Note taking is a key part of documenting the outputs of the symposium. If you’re elected to be the note taker, be creative. You can take notes on a flip chart, sticky notes or electronically in Google doc, Google Draw or other document-sharing application. Notes will be archived and shared publicly after the symposium.
Wrap up the session at 12:30. After lunch, you’ll return to your group to create the action plan.
3. The Action Plan
In this 40 minute session, your group will reconvene to set out a plan of action.
To help plan your next steps and prepare your report to present back to everyone, each group write a postcard to themselves. Imagine receiving this postcard sometime in the future (the group sets the date). Keep your action plan reasonable and doable.
- Where did we start? (Describe the world as it is today)
- Where are we now? (Describe what it will be in the future.)
- How did we get here? (What happened? What steps did you take to get to the future state?
- Who led this effort? (What group/person/network led the charge?)
See this sample postcard to the future from an event from 2014.
Thank to Marlies van Dijk, RN, MSc to this sample and her unconference wisdom.
Choose a person from your group to report your action plan back to all the symposium attendees.
4. Solutions Exchange
With everyone back in the main room, each group has 2 minutes to present their action plan.
As Pat Rich said, this is #hcsmca’s not so hidden agenda. These action plans will usher #hcsmca into it’s next phase of social collaboration and innovation.
For the final word, Kathy Kastner shares what to expect at an unconference in 3 Cs.